Employers can expect another large hit to their budget next year from the soaring cost of providing employee health benefits, according to two new reports.
Based on a survey of 450 employers, Willis Towers Watson expects benefit costs in 2024 to rise by 6%, slightly higher than the 5.7% jump it predicted for 2023. Meanwhile, Mercer’s 2023 National Survey of Employer-Sponsored Health Plans suggests a 5.4% increase next year—similar to the level it forecast for 2023, according to its survey of more than 1,700 employers across the nation.
These predictions are in stark contrast to the average annual increase of 3%-4% for employer health benefit costs that have been typical for most of the past decade, according to Mercer.
In addition to recent inflationary pressures, says Sunit Patel, chief actuary for health and benefits for Mercer, “the consolidation of health systems and the introduction of ultra-expensive gene and cellular therapies” are among the systemic forces boosting costs.
Alan Silver, senior director and financial, analytics and actuarial intellectual capital leader at WTW, points to other issues driving costs.
Employers, for example, are seeing greater employee demand for and use of expensive prescription drugs; some of these are needed because long-term illness went unchecked during the pandemic, leading to a rise in diagnoses like cancer in particular, Silver told HRE. When such conditions are caught earlier, the employer costs are less in the long run.
Also, earlier this year, employers started to see a surge in interest from employees in costly GLP-1 semaglutide drugs for diabetes and obesity, including Ozempic and Wegovy, he notes. Despite the expense, more employers are expected to cover the cost of weight loss drugs next year.
Employers eat the cost increase
Rather than pass the cost increase to their workforce, employers are biting the bullet once again and absorbing the added expense, the Mercer report shows.
According to the survey, large employers with a workforce of 500 or more people have avoided shifting rising healthcare costs to employees for the past five years. This assessment is based on minimal growth in deductibles and other cost-sharing measures, the report states.
During the pandemic, a number of employees faced greater financial strain from partners and spouses getting laid off and a decline in household income, leading many employers to shoulder these rising costs, a Mercer blog post points out.
Instead of mitigating the cost by passing it on to workers, a number of employers are implementing cost-management strategies, especially related to complex care and chronic medical conditions—two of the biggest drivers of healthcare costs, the report states.
For example, 84% of employers with 500 or more employees list managing high-cost claimants as an important cost-management strategy for the next three to five years, with 52% of those saying it is very important.
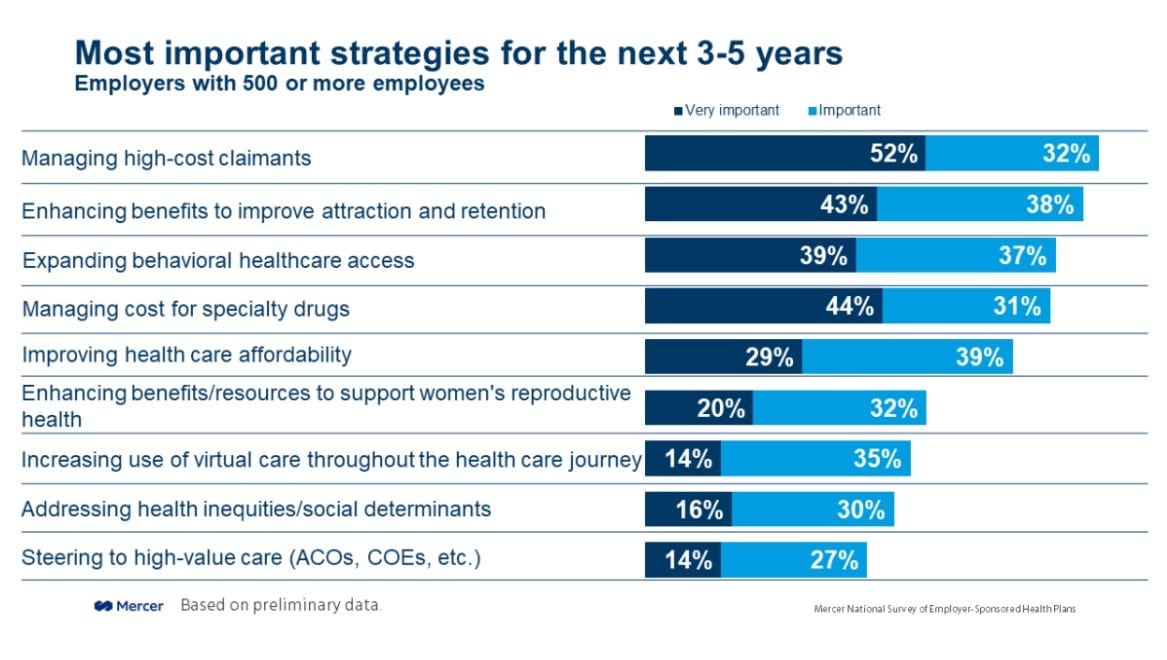 Meanwhile, large employers are also adding Centers of Excellence to their health plan networks. These are designed to connect employees needing complex care to providers and resources specific to their illness. More than a quarter (28%) of large employers also offer healthcare navigation to point employees to the best provider quickly. By taking these measures and others, employers may see better outcomes for their employee patients, which ultimately can save an employer money.
Meanwhile, large employers are also adding Centers of Excellence to their health plan networks. These are designed to connect employees needing complex care to providers and resources specific to their illness. More than a quarter (28%) of large employers also offer healthcare navigation to point employees to the best provider quickly. By taking these measures and others, employers may see better outcomes for their employee patients, which ultimately can save an employer money.
Are 6% health benefit cost increases the new normal?
As hybrid work has become the new normal in corporate America, can the same be said for the lofty 6% annual increases in health benefit costs?
Beth Umland, director of research for Mercer’s health & benefits business, told HRE that the cost increase directly reflects the events of the last few years. These include high inflation and the tight labor market, she says.
In particular, the healthcare industry and hospital systems may continue to experience a talent shortage that will drive up operations costs, which they need to pass on.
However, Silver predicts employers may see a cost reprieve in the future. He still suggests that HR leaders keep an eye on the changing landscape, though.
“We think that depends on how employers respond to this environment. It is reasonable to believe that the price aspect of this increase may be shorter-lived if the inflationary environment stabilizes,” Silver says. “That said, there are even more gene therapy prescription drugs and other potential concerns about utilization that need to be mitigated to change the cost curve.”

